Discover how your microbiome influences spinal disc integrity—& practical strategies to prevent back pain

In recent years, scientific research has increasingly highlighted the importance of gut health and its far-reaching impacts on various bodily functions. Terms like the "gut-brain axis" and the "gut-skin axis" have entered mainstream discussions, emphasizing how the microbiota within our intestines can influence our mental health and skin conditions, respectively. Another fascinating and relatively lesser-known connection is the gut-disc axis, which explores the relationship between gut health and spinal disc health. This comprehensive guide delves into the intricacies of the gut-disc axis, shedding light on how gut microbiota can impact spinal health and offering practical advice for maintaining a healthy gut to prevent disc-related issues.
The gut microbiota: An overview
What are gut microbiota?
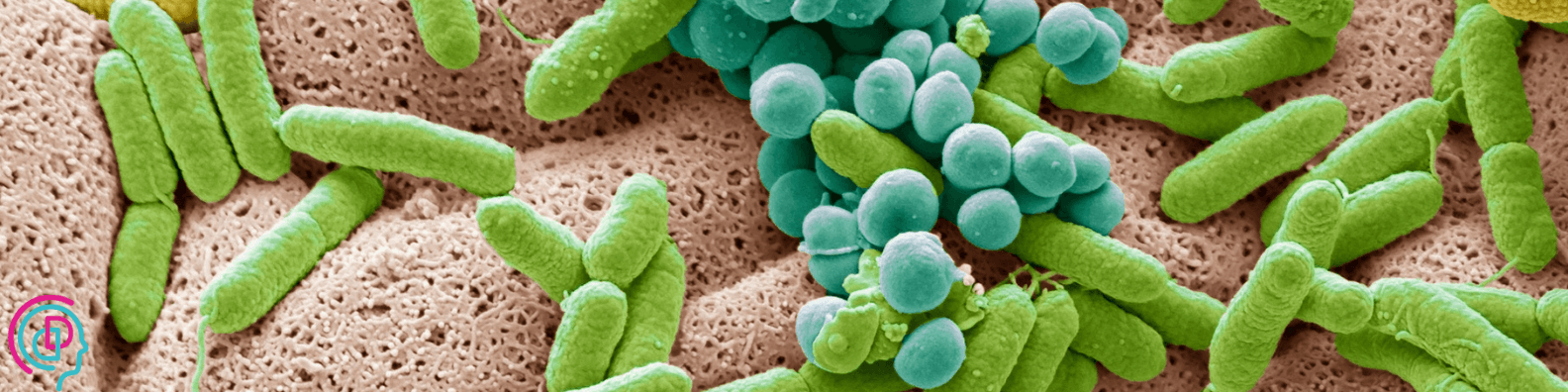
The human gut is home to trillions of microorganisms, collectively known as the gut microbiota. These microorganisms include bacteria, fungi, and other microbes, which coexist symbiotically within our digestive tract. The gut microbiota plays a crucial role in digestion, nutrient absorption, immune function, and the synthesis of essential vitamins.
What is the gut microbiome?
The gut microbiome encompasses the gut microbiota along with their genetic material and the surrounding environmental conditions. It includes not only the microorganisms themselves but also their genomes and the molecules they produce, such as metabolites. The microbiome reflects the broader ecological and functional aspects of the microbial community within the gut.
The role of gut microbiota in inflammation
One of the primary functions of the gut microbiota is to maintain a balanced immune response. A healthy gut microbiota helps to regulate inflammation by controlling the production of pro-inflammatory and anti-inflammatory compounds. However, when the balance of these microorganisms is disrupted—a condition known as dysbiosis—it can lead to chronic inflammation, which is linked to a variety of health issues, including autoimmune diseases, metabolic disorders, and even mental health conditions.
The spinal discs: Structure & function
Anatomy of spinal discs
The spinal column is composed of 24 vertebrae, which are separated by intervertebral discs. These discs act as shock absorbers, cushioning the vertebrae and allowing for flexibility and movement. Each intervertebral disc consists of two main components: the annulus fibrosus and the nucleus pulposus. The annulus fibrosus is the tough, outer layer made of collagen fibers, while the nucleus pulposus is the gel-like core that provides elasticity and absorbs impact.
Common spinal disc problems
Spinal discs are prone to various issues, such as herniation, degeneration, and lumbago.
- Herniated discs: Occur when the nucleus pulposus protrudes through a tear in the annulus fibrosus, potentially compressing nearby nerves and causing pain. This pain can manifest in various ways, including lower back pain, leg pain, or localized pain in areas like the knee or foot.
- Degenerative disc disease: Involves the gradual breakdown of the discs over time, leading to chronic pain and reduced mobility.
- Lumbago: Or lower back pain, often associated with disc problems and significantly impacting quality of life.
The gut-disc axis: Exploring the connection
Inflammation & spinal disc health
The link between gut health and spinal disc health primarily revolves around inflammation. Chronic inflammation in the gut, often resulting from dysbiosis, can contribute to systemic inflammation. This systemic inflammation can affect various tissues and organs, including the spinal discs. Research suggests that inflammatory cytokines produced in the gut can travel through the bloodstream and reach the spinal discs, exacerbating existing disc issues or even contributing to their development.
Gut dysbiosis & disc degeneration
Emerging evidence indicates that gut dysbiosis may play a role in the degeneration of spinal discs. Dysbiosis can lead to an overproduction of pro-inflammatory cytokines and a decrease in anti-inflammatory compounds, creating an environment that promotes disc degeneration. Additionally, dysbiosis can impair nutrient absorption, depriving the spinal discs of essential nutrients required for their maintenance and repair.
The microbiota-spine connection: Key studies
Recent studies have explored the concept of the "gut-disc axis," suggesting a potential link between gut microbiota and intervertebral disc health, including conditions such as lumbar herniation. The gut-disc axis theory posits that gut microbes can influence the microenvironment of intervertebral discs (IVD) through various mechanisms, such as immune modulation, metabolite production, and inflammation regulation.
Mechanisms of influence
- Immune modulation: Gut microbiota can influence the systemic immune response, potentially affecting inflammation levels within the IVDs. Dysbiosis may lead to chronic low-grade inflammation, contributing to disc degeneration and herniation.
- Metabolite production: Microbes in the gut produce metabolites like short-chain fatty acids (SCFAs), which can reach the IVDs and influence disc health by modifying the local microenvironment.
- Barrier function and inflammation: Increased intestinal permeability ("leaky gut") allows bacterial products to enter circulation, triggering systemic inflammation that may affect IVD integrity.
Research evidence
- A Mendelian randomization study found associations between gut microbiota composition and risk of disc degeneration and low back pain.
- Reviews highlight gut dysbiosis leading to systemic inflammation, exacerbating disc degeneration and pain.
- Evidence suggests a unique microbiome within IVDs, with dysbiosis influencing disc health directly.
- Clinical findings show altered gut microbial diversity and increased inflammatory cytokines (e.g., TNF-α, IL-1β) in patients with lumbar disc degeneration.
Practical strategies for maintaining a healthy gut

Diet & nutrition
A balanced diet rich in fiber, probiotics, and prebiotics supports gut microbiota. Include fruits, vegetables, whole grains, legumes, yogurt, kefir, sauerkraut, and kimchi. Prebiotics like garlic, onions, and bananas feed beneficial bacteria, promoting gut balance.
Lifestyle factors
Regular exercise promotes microbial diversity, while excessive alcohol and smoking disrupt gut balance. Stress management through mindfulness, meditation, and adequate sleep reduces inflammation.
Supplements & medications
Probiotic and prebiotic supplements can help maintain gut health, especially when diet alone isn’t enough. When using antibiotics, co-administration of probiotics may mitigate gut disruption.
Preventing spinal disc issues through gut health

Anti-inflammatory diet
An anti-inflammatory diet—rich in antioxidants and omega-3s—can reduce systemic inflammation. Emphasize fatty fish, nuts, seeds, leafy greens, and berries.
Hydration & exercise
Adequate hydration keeps discs supple. Exercises like yoga and Pilates enhance spinal flexibility and core strength.
Stress reduction techniques
Stress reduction supports gut and spinal health. Practices like deep breathing, progressive muscle relaxation, and time in nature help lower stress.

Conclusion: The future of gut-disc axis research
The emerging field of the gut-disc axis promises new insights into gut–spine interactions. Prioritizing gut health through diet, lifestyle, and supplements may aid spinal health. Future therapies may target the microbiome to prevent or treat disc degeneration.
Embracing a holistic approach
Recognizing the interconnectedness of bodily systems is key. Maintaining a balanced gut microbiota can prevent and manage spinal disc issues.
Looking ahead
As research advances, targeted interventions to modulate the gut microbiome for spinal health are anticipated. In the meantime, healthy lifestyle and dietary choices remain essential.
Sources
- Li et al. “Gut-disc axis: A cause of intervertebral disc degeneration and low back pain?” Eur Spine J (2022). https://doi.org/10.1007/s00586-022-07152-8
- Geng et al. “Gut microbiota and intervertebral disc degeneration…” J Orthop Surg Res (2023). https://doi.org/10.1186/s13018-023-04081-0
- Fang et al. “Causal associations between gut microbiota…” Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08131-x
- Rajasekaran et al. “Human intervertebral discs harbour a unique microbiome…” Eur Spine J (2020). https://doi.org/10.1007/s00586-020-06446-z
- Lin et al. “Propionibacterium acnes induces intervertebral disc degeneration…” Emerg Microbes Infect (2018). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5837142/



























0 Comments